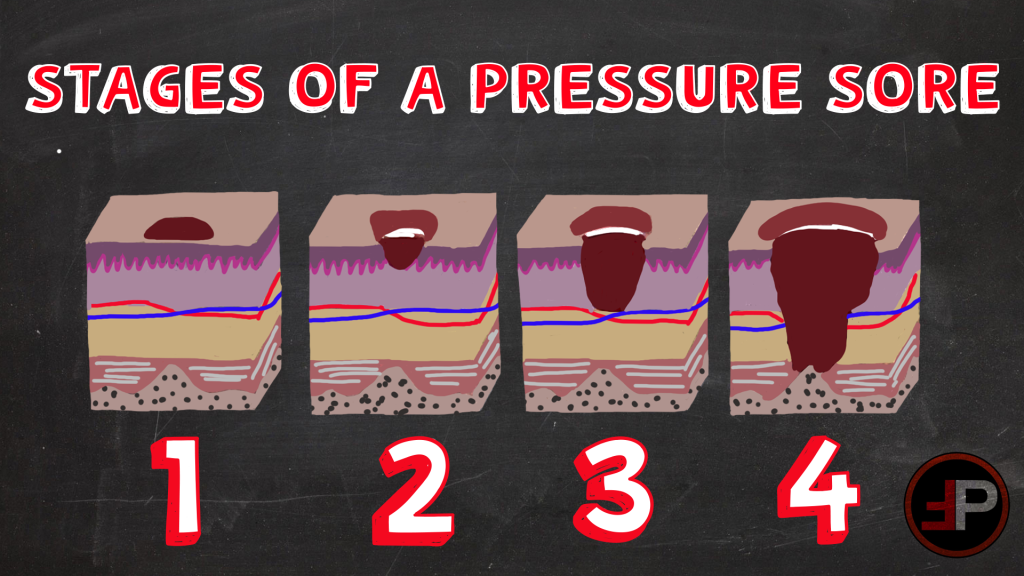
You just bought yourself an awesome, new pair of shoes. So, what do you do next? Break them in of course! 20 minutes later you notice an open blister on your heel from where your shoes were rubbing a little too hard. That my friends is a stage 2 sheer-related pressure injury (PI). And to think, if the skin was still intact it would be a stage 1.

Why am I telling you this? It is in hopes to relate to you how easy it is for our patients to get PIs. Even deep tissue injuries, stage 3 and 4, can occur in as few as one to two hours. And these injuries aren’t just a bad mark on a hospital’s record, it has financial repercussions for patients as well. There is an associated increased length of stay and a cost of over $40,000. YIKES!
“But I’m not in the hospital, what do PIs have to do with me? Is there anything I can do?” Yes, definitely, absolutely! Those are great questions. This article is here to help ease some of the PI FAQs that are relevant to the pre-hospital world of transportation.
What are Pressure Injuries?
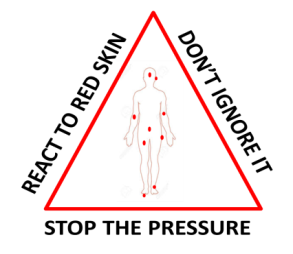
PIs are localized damage to the skin and/or underlying soft tissue, usually over a bony prominence or related to medical or other devices. These injuries, according to the Joint Commission, are mostly preventable. They can develop in less than an hour and can take up to three days to present. And while there are studies that show most acute care patient PIs are preventable, there has been no significant evidence of the same to show this is true for critical care patients.
What Affects Pressure Injuries?
A mix of intrinsic and extrinsic factors can cause great concern for PI development. The three types of factors are static intrinsic, dynamic intrinsic, and dynamic extrinsic. Static intrinsic factors are traits that patients have that cannot be changed: age, smoking, renal failure. Dynamic intrinsic factors are traits patients have that can change, such as hemodynamics, hypoxia, initial injury, and shock. Lastly, dynamic extrinsic factors are those that are typically treatment-related: vasopressors, ICU stay, chemical-induced paralysis, and medical devices. These all lead to impaired tissue tolerance, perfusion to the skin, and pressure and friction.
Critical Care Risk Factors
Critical Care patients are a special population who have many factors affecting their tissue tolerance, perfusion, pressure, shear, and microclimate. Critical care patients tend to need a little external help from machines and medication to get better. CRRT, ECMO, mechanical ventilation, IABPs, VADs, diabetes, vascular disease, and vasopressors are factors to be aware of when thinking about patients at high risk of developing PIs during transport. A specific vasopressor combination shown to increase PIs is norepinephrine and vasopressin.
PI Prevention
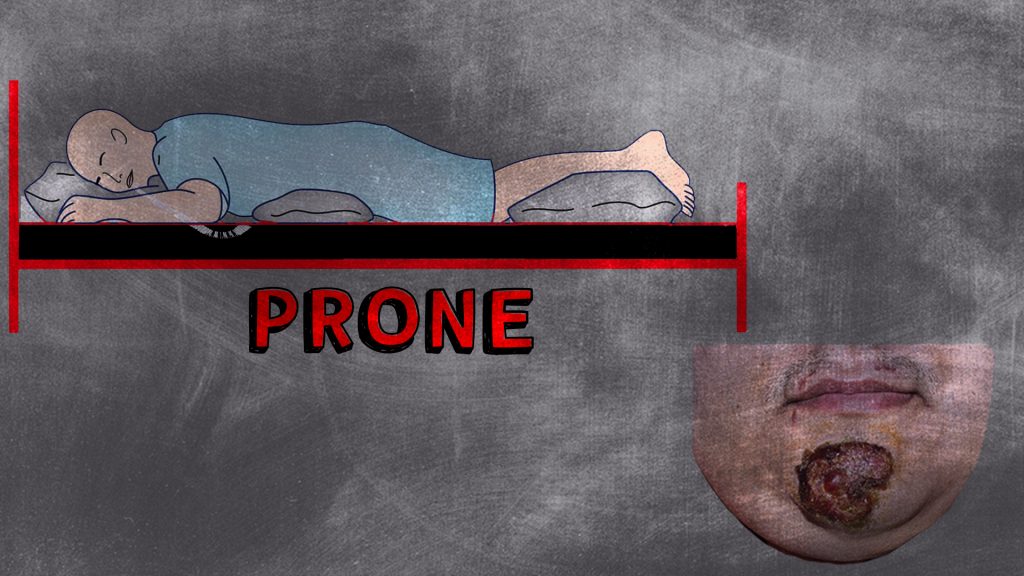
“But I can’t turn my patient in an [insert transportation method]”. Now that we have that out of the way, let’s talk about other things we can do in the pre-hospital or hospital world. First I would like to mention that the recommendation of turning and repositioning a patient every two hours lacks evidence. So feel confident in knowing that having a supine-positioned patient on a two-hour transport may not be the reason for a PI that happens. Things we do affect are; pressure-causing devices, hemodynamic stability, oxygenation, and even stretcher sheet choice (ooh la la).
Making sure we position our devices to keep pressure off the patient, such as foam dressings and fluidized positioners, can help reduce injury to an area that may already have integrity issues. Stabilizing hemodynamics will also help the integrity by ensuring oxygenation to the skin. The same goes for the choices and usage of vasopressors, although ultimately patient condition takes precedence over PI prevention. Lastly, silk-like sheets are shown in one study to be the best sheet choice because it causes less shear injury, provide a more comfortable microclimate with some moisture-wicking properties, and have been shown to decrease acquired PIs in the ICU population.

What’s Next?
We have all heard that standard stretcher mattresses are for CPR, not comfort. This along with needing to be able to take a beating that comes with being part of EMS equipment as well as harsh cleanings multiple times a shift could be the reason they are usually made from foam and a hard plastic covering. Although, PI Panels suggest using a “redistributing support surface during transport”.
A random study found that alternating pressure overlays and alternating pressure mattresses aided in developing new and healing existing PIs. As of right now, there are no commercial products available. Overlays could be fitted to stretcher mattresses but could be unsafe due to the added height possibly exceeding the height of the side rails. Another factor would be the added need for power in an ambulance or aircraft that is already powering a number of other devices including the monitor, batteries, fridge, pumps, etc.
Although maybe we could find a solution in the near future as devices become smaller and medicine and technology advance. Until then, we can spread awareness about PI prevention in transports and do what we can to help keep our patient’s skin, unlike our sanity, intact.
REFERENCES
Agency for Healthcare Research and Quality. (2014, Oct). Preventing pressure ulcers in hospitals. Retrieved from https://www.ahrq.gov/patient-safety/settings/hospital/resource/ pressureulcer/tool/pu1.html#:~:text=Cost%3A%20Pressure%20ulcers%20cost%20%249.1,related%20to%2 0pressure%20ulcers%20annually.
Barella, David and Downie, Fiona (2021) Pressure redistribution in the ambulance: is this possible? Wounds UK, 17 (3). pp. 66-71. ISSN 1746-6814.
Cox, J. (2022, Aug. 11). Vasopressors and pressure injury risk in the critically ill [Webinar]. American Association of Critical-Care Nurses. https://www.aacn.org//education/webinar- series/wb0068/vasopressors-and-pressure-injury-risk-in-the-critically-ill
Dukes, Susan F., et al. “Pressure Injury Development in Patients Treated by Critical Care Air Transport Teams: A Case-Control Study.” Critical Care Nurse, vol. 38, no. 2, 1 Apr. 2018, pp. 30–36., https://doi.org/10.4037/ccn2018993.
The Joint Commission. (2022, Mar.). Quick Safety Issue 25: Preventing pressure injuries. Retrieved from https://www.jointcommission.org/resources/news-and-multimedia/ newsletters/newsletters/quick-safety/quick-safety-issue-25-preventing-pressure-injuries/

